Heat transfer from the body occurs through the pituitary gland and the salivary glands. The importance of endocrine glands for humans.
The regulation of the physiological functions of the body is carried out using two systems - nervous and humoral. In the body they act in concert. Nervous regulation is carried out quickly, in a split second, humoral regulation - slowly. This type of regulation is limited by the speed of blood movement through the vessels (0.005-0.5 m/s). Nervous and humoral regulation are closely related to each other and carry out a single neurohumoral regulation. Central nervous system, including its senior department- cerebral cortex, regulates gland functions internal secretion. This is done by transmitting nerve impulses directly to organs and tissues. Humoral regulation involves the regulating influence of biologically transported blood, lymph, tissue fluid active substances.
Glands that do not have excretory ducts and secrete their secretions (hormones) directly into the tissue fluid and blood are called endocrine(Fig. 193).
The process of production and release of active substances by endocrine glands is called internal secretion, and the substances are called hormones.
Hormones- chemical compounds with high biological activity, in small doses, give a significant physiological effect. By chemical composition distinguish: 1) steroid hormones; 2) proteins and peptides; 3) derivatives of amino acids.
Hormones are characterized by:
1) distant action. The organs and systems on which hormones act are located far from the place of their formation in endocrine glands Oh;
2) strict specificity of action. The reaction of organs and tissues to hormones is strictly specific. The specificity of the action of hormones is ensured by the presence of receptor molecules in cells. Only organ cells have receptors for the corresponding hormone.
Rice. 193.Location of endocrine glands (diagram)1 - pineal body;2 - pituitary gland; 3 - thyroid and parathyroid glands;4 - thymus gland (thymus);5 - adrenal gland; 6 - islet part of the pancreas;7 - intrasecretory part of the testicles (in men);8 - intrasecretory part of the ovary (in women).
on-targets, capable of reading chemically encoded information due to this;
3) high biological activity. Hormones are produced by endocrine glands in very small quantities.
Hormones are involved in the regulation and integration of all body functions. They contribute to the body’s adaptation to changing conditions of the external and internal environment and restore the altered balance of the internal environment.
The endocrine glands have different locations, but they are closely related to each other. Violation of the function of one leads to changes in the activity of others. A certain level of hormones is required for the body to function. The lack of one or another hormone indicates a decrease in activity (hypofunction) of this gland, excess - about increased activity (hyperfunction).
With hypo- and hyperfunction of the glands, various endocrine diseases.
The endocrine glands are abundantly supplied with blood and lymphatic vessels. Vegetative fibers are suitable for them nervous system.
Endocrine glands are divided into dependent and independent from the anterior lobe pituitary gland
To the glands dependent on the pituitary gland include thyroid gland cortical substance of the adrenal glands gonads. The relationship between the anterior lobe of the pituitary gland and these glands is based on the type of direct and feedback connections.
Tropic hormonesthe anterior lobe of the pituitary gland activates the activity of the glands. Gland hormones, acting on the anterior lobe of the pituitary gland, inhibit the formation and release of the corresponding hormone.
TO independent of the anterior lobe pituitary gland include parathyroid glands, pineal gland, pancreatic islets(islets of Langerhans of the pancreas), adrenal medulla, paraganglia.
The highest center for the regulation of endocrine functions is hypothalamus(division of the diencephalon). It unites non-
regulating and endocrine mechanisms of regulation into the general neuroendocrine system. The hypothalamus forms a single functional complex with the pituitary gland. The hypothalamus contains neurons of the usual type and neurosecretory cells. Both types of cells produce protein secretions and mediators. In neurosecretory cells, protein synthesis predominates, and neurosecretion is released into the blood. Thus, the nerve impulse is converted into a neurohumoral one.
Pituitary
Pituitary(brain appendage) - a small gland weighing 0.5-0.7 g. Located in the pituitary fossa of the sella turcica of the sphenoid bone. Through an opening in the diaphragm of the sella, the pituitary gland is connected to the infundibulum of the hypothalamus of the diencephalon. The pituitary gland consists of three lobes: front(adenohypophysis), intermediate And rear(neurohypophysis).
IN anterior lobe The pituitary gland produces a number of hormones: somatotropic, thyrotropic, gonadotropic, adrenocorticotropic and others.
Somatotropicthe hormone controls the growth of bones, muscles, organs, regulates metabolic processes in organism.
At hyperfunction V childhood arises gigantism(Fig. 194), in an adult - acromegaly(enlargement of individual parts of the body: arms, legs, nose, etc.) (Fig. 195). At hypofunction in childhood a person remains a dwarf. Pituitary dwarfs have normal mental development and correct body proportions (Fig. 194). Hypofunction in adults causes changes in metabolism, which leads to either general obesity, or to sudden weight loss.
Thyroid-stimulating hormone controls the function thyroid gland, affects its development and hormone production.
Adrenocorticotropic hormone regulates functions cortical substances adrenal glands
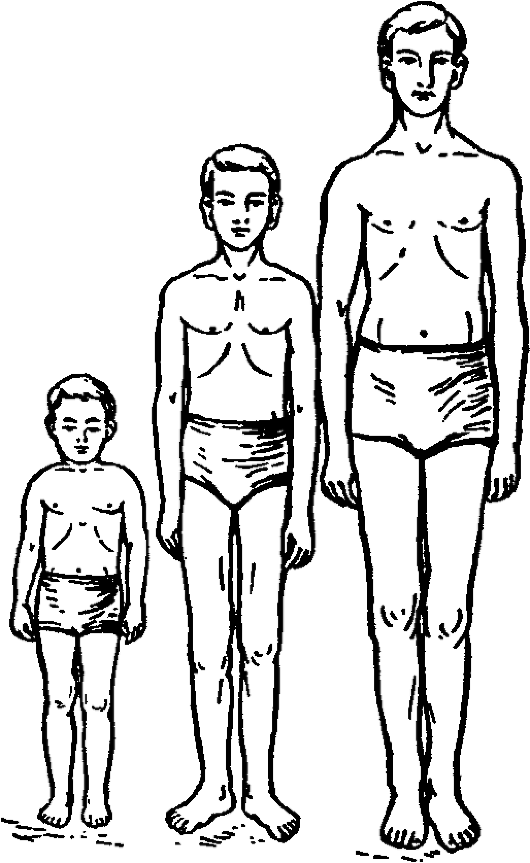
Rice. 194.Gigantism. The boys are the same age (14 years old). On the left is a pituitary dwarf - height 100 cm; on the right - pituitary giant - height 187 cm; in the center - a normal boy - height 148 cm.
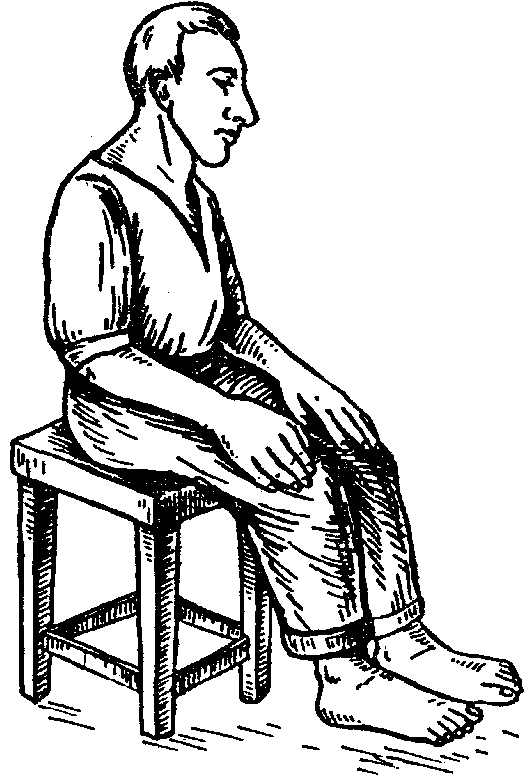
Rice. 195.Patient with acromegaly. Overgrowth of the lower jaw, nose, hands and feet.
TO gonadotropic hormones include follicle-stimulating(promotes the growth of germ cells), luteinizing(increases the formation of sex hormones and growth corpus luteum), luteotropic (promotes the formation of the corpus luteum and the synthesis of progesterone), prolactin(increases milk production by the mammary glands).
Intermediate part the anterior pituitary gland secretes hormones melanocytotropin, regulating the synthesis of melanin pigment, and lipotropin, activating fat metabolism.
Posterior pituitary gland (neurohypophysis) formed nerve tissue, does not synthesize hormones. Biologically active substances are transported to the posterior lobe of the pituitary gland oxytocin And vasopressin. They are produced by the nuclei of the hypothalamus, accumulate in the pituitary gland and are released into the blood. Vasopressin has a vasoconstrictor and antidiuretic effect.
Oxytocinacts on the smooth muscles of the uterus, enhancing its contractions at the end of pregnancy, and stimulates milk secretion.
Thyroid
Thyroid located on the neck in front of the larynx. It has two lobes and an isthmus. The weight of the gland in an adult is 20-30 g. The gland is covered on the outside with a connecting capsule, which divides the organ into lobules.
Slicesconsist of vesicles (follicles), which are structural and functional units. The thyroid gland produces iodine-rich hormones thyroxine And triiodothyronine. Their main function is to stimulate oxidative processes in the cell. Hormones affect water, protein, carbohydrate, fat, mineral metabolism, growth, development and differentiation of tissues. They affect the functions of the central nervous system and higher nervous activity.
Hormone thyrocalcitonin participates in the exchange of calcium and phosphorus, reducing the calcium content in the blood and the reabsorption of calcium from the bones.

Rice. 196.Graves' disease, characterized by exophthalmos. The patient before surgery (left) and after surgery (right).
At hyperfunction thyroid gland occurs Graves' disease(enlarged thyroid gland, increased excitability of the nervous system, basal metabolism, bulging eyes (exophthalmos), decreased body weight) (Fig. 196).
At hypofunction of the gland occurs in childhood cretinism(stunted growth, mental and sexual development). With hypofunction, an adult develops myxedema(decreased basal metabolism, obesity, apathy, decreased body temperature, mucous swelling fabrics).
At iodine deficiency people suffer in water endemic goiter(secreting tissue grows in the thyroid gland).
Parathyroid glands
Parathyroid glands (upper and lower) are located on back surface lobes of the thyroid gland. Their number can vary from 2 to 8. The total mass of the parathyroid gland in an adult is from 0.2-0.35 g. The epithelial cells of these glands produce parathyroid hormone, involved in the metabolism of calcium and phosphorus in the body.
It promotes the release of calcium and phosphorus ions from bones into the blood. Parathyroid hormone enhances the reabsorption of calcium by the kidneys, reducing the excretion of calcium in the urine and increasing its content in the blood.
Adrenal glands
Adrenal glands- paired organs located retroperitoneally directly above the upper poles of the kidneys. The mass of one adrenal gland in an adult is about 12-13 g. They consist of two layers: outdoor(cortical) and internal(cerebral).
IN cortex three groups of hormones are produced: glucocorticoids, mineralocorticoids And sex hormones.
Glucocorticoids (hydrocortisone, corticosterone and etc.) affect the metabolism of carbohydrates, proteins, fats, stimulate the synthesis of glycogen from glucose, and have an anti-inflammatory effect. Glucocorticoids ensure the body's adaptation to emergency conditions.
Mineralocorticoids (aldosterone, etc.) regulate the exchange of sodium and potassium, acting on the kidneys. Aldosterone enhances the reabsorption of sodium into renal tubules, enhances potassium secretion, participates in the regulation water-salt metabolism, tone of blood vessels, helps to increase blood pressure.
Sex hormones (androgens, estrogens, progesterone) ensure the development of secondary sexual characteristics.
At hyperfunction adrenal glands increase the synthesis of hormones, especially sex hormones. At the same time, secondary sexual characteristics change (women develop a beard, mustache, etc.).
At hypofunction develops bronze disease. The skin acquires a bronze color, loss of appetite, increased fatigue, nausea, and vomiting are observed.
Medullaadrenal glands secretes adrenalin And norepinephrine, participating in carbohydrate metabolism and affecting the cardiovascular system.
Adrenalinincreases systolic blood pressure and cardiac output, increases heart rate, and dilates coronary vessels.
Norepinephrinereduces heart rate and cardiac output.
Endocrine part of the pancreas
The endocrine part of the pancreas is represented by islets of Langerhans. The largest number of them is located in the tail of the pancreas. β cells islets produce the hormone insulin, and α cells- glucagon. These hormones have the opposite effect. Insulin promotes the transformation glucose V glycogen, reduces blood sugar levels, enhances carbohydrate metabolism in muscles, etc. Glucagon is involved in the conversion of glycogen into glucose in the liver, resulting in increased blood sugar levels.
D cellssecrete a hormone somatostatin. Somatostatin inhibits the production of growth hormone, as well as the release of insulin and glucagon by α- and β-cells.
At insufficient secretion of hormones by the gland develops diabetes. With this disease, tissues do not absorb glucose, its content in the blood and excretion in urine increases.
Endocrine part of the gonads
Sex glands(testis and ovary) produce sex hormones. IN testes male sex hormones are produced - androgens: (testosterone n) and androsterone. Androgens influence embryonic differentiation and development of reproductive organs, puberty, spermatogenesis, development of secondary sexual characteristics, sexual behavior. These hormones stimulate protein synthesis and accelerate tissue growth.
Female sex hormones are synthesized in the ovary - estrogens(folliculin) And progesterone, which is produced by the cells of the corpus luteum. In addition, small amounts of androgens are produced in the ovaries. Estrogens influence the development of the external genitalia, secondary sexual characteristics, growth and development of the musculoskeletal system, ensuring the development of the body according to the female type. Progesterone prepares the uterine mucosa for implantation of the embryo, affects the development of the placenta and mammary glands, delays the development of new follicles, etc.
Pineal gland
pineal body, or pineal gland of the brain, part of the diencephalon (epithalamus) also performs endocrine functions. The epiphysis is located in the groove between the superior colliculi of the midbrain quadrigeminal. Its mass is about 0.2 g.
The pineal gland secretes a hormone melatonin, inhibiting the action of gonadotropic hormones. The secretion of the pineal gland changes depending on the light: light inhibits the synthesis of melatonin. The effect of light is realized with the participation of the hypothalamus.
The pineal gland regulates the function of the gonads and puberty. After removal of the epiphysis, premature puberty occurs.
Questions for self-control
1. What systems regulate the physiological functions of the body?
2. How is humoral regulation carried out?
3. Which glands are called endocrine?
4. What are hormones?
5. What are the characteristics of hormones?
6. What processes are hormones involved in?
7. What occurs with hyper- and hypofunction of the endocrine glands?
8. Which glands depend on the pituitary gland?
9. Which glands do not depend on the pituitary gland?
10. What is the highest center for the regulation of endocrine functions?
11. What is the structure of the pituitary gland?
12. What hormones are produced by the anterior pituitary gland?
13. What diseases occur with hyper- and hypofunction of somatotropic hormone of the anterior pituitary gland?
14. What hormones are produced by the intermediate lobe of the pituitary gland?
15. Where are neurohypophysis hormones produced?
16. Where is it located? thyroid?
17. What hormones does the thyroid gland produce?
18. What do thyroid hormones affect?
19. What diseases occur with hyper- and hypofunction of the thyroid gland?
20. Where are the parathyroid glands located?
21. What hormone do the parathyroid glands secrete?
22. Where are the adrenal glands located?
23. What hormones are produced in the adrenal cortex?
24. What do glucocorticoids affect?
25. What do mineralocorticoids regulate?
26. What do adrenal sex hormones influence?
27. What occurs with hyper- and hypofunction of the adrenal cortex?
28. What hormones are produced by the adrenal medulla?
29. What is the endocrine part of the pancreas represented by?
30. What cells produce insulin?
31. What cells produce glucagon?
32. In what processes are insulin and glucagon involved?
33. What cells secrete somatostatin?
34. What disease develops with insufficient insulin secretion?
35. What hormones are produced in the testes?
36. What hormones are produced in the ovaries?
37. What processes are affected by female hormones?
38. What processes are affected by male hormones?
39. Where is the pineal gland located?
40. What hormones does the pineal gland secrete?
41. What functions is it involved in regulating?
Keywords of the topic “Endocrine glands”
Islet D cells
adenohypophysis
adrenalin
adrenocorticotropic hormone
islet α cells
acromegaly
aldosterone
amino acids
androgens
androsterone
Graves' disease
biological activity
bronze disease
vasopressin
Islet β cells
gigantism
hydrocortisone
hyperfunction
hypothalamus
pituitary
hypofunction
glycogen
glucagon
glucose
glucocorticoids gonadotropic hormone hormones
endocrine glands
corpus luteum
insulin
calcium
dwarf
corticosterone cortex cretinism lipotropin
luteinizing hormone
melanin
melanocytropin
melatatin
metabolism
myxedema
mineralocorticoids
medulla
adrenal glands
neurohypophysis
neuron
neurosecret
neuroendocrine system nerve impulses norepinephrine oxytacin basal metabolism islets of Langerhans parathyroid hormone parathyroid glands peptides
pancreas
gonads
progesterone
prolactin
goggle-eyed
thyrocalcitonin
growth hormone
diabetes
secret
testis
mucous tissue swelling
somatostatin
specificity of action
steroid hormones
testosterone
thyroxine
tropic hormones
triiodothyronine
carbohydrates
follicle stimulating hormone phosphorus
thyroid
endocrine glands
pineal gland
estrogens
Physiology of internal secretion- a section that studies the patterns of synthesis, secretion, transport of physiologically active substances and the mechanisms of their action on the body.
Liberins and statins
Regulation of the secretion of pituitary hormones
Triple hormones (ACTH, TSH, FSH, LH, LTG)
Regulation of the activity of the thyroid, gonads and adrenal glands
A growth hormone
Regulation of body growth, stimulation of protein synthesis
Vasopressin (antidiuretic hormone)
Affects the intensity of urination by regulating the amount of water released by the body
Thyroid (iodine-containing) hormones - thyroxine, etc.
Increases the intensity of energy metabolism and body growth, stimulation of reflexes
Calcitonin
Controls calcium metabolism in the body, “saving” it in the bones
Parathyroid hormone
Regulates blood calcium levels
Pancreas (islets of Langerhans)
Reducing blood glucose levels, stimulating the liver to convert glucose into glycogen for storage, accelerating the transport of glucose into cells (except nerve cells)
Glucagon
Increasing blood glucose levels stimulates the rapid breakdown of glycogen into glucose in the liver and the conversion of proteins and fats into glucose
Brain sleep:
- Adrenalin
- Norepinephrine
Increased blood glucose levels (receipt from the liver to cover energy costs); stimulates heart rate, accelerates breathing and increases blood pressure
Cortical layer
- Glucocorticoids (cortisone)
A simultaneous increase in blood glucose and glycogen synthesis in the liver affects 10 fatty and protein metabolism(protein decoupling) Stress resistance, anti-inflammatory effect
- Aldosterone
Increased sodium in the blood, fluid retention in the body, increased blood pressure
Sex glands
Estrogens/female sex hormones), androgens (male sex hormones)
Provide sexual function of the body, development of secondary sexual characteristics
Properties, classification, synthesis and transport of hormones
Hormones- substances secreted by specialized endocrine cells of the endocrine glands into the blood and having a specific effect on target tissues. Target tissues are tissues that are very sensitive to certain hormones. For example, for testosterone (male sex hormone) the target organ is the testes, and for oxytocin - the myoepithelium of the mammary glands and the smooth muscles of the uterus.
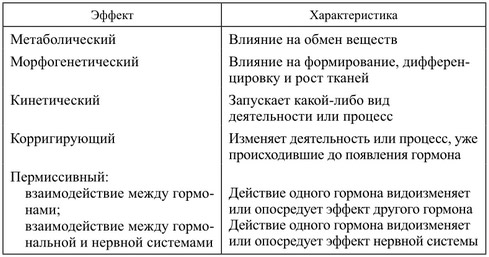
Hormones can have several effects on the body:
- metabolic effect, manifested in a change in the activity of enzyme synthesis in the cell and in an increase in the permeability of cell membranes for this hormone. At the same time, metabolism in tissues and target organs changes;
- morphogenetic effect, which consists in stimulating growth, differentiation and metamorphosis of the organism. In this case, changes occur in the body at the genetic level;
- kinetic effect consists in activating certain activities of executive bodies;
- corrective effect manifested by a change in the intensity of the functions of organs and tissues even in the absence of the hormone;
- reactogenic effect associated with changes in tissue reactivity to the action of other hormones.
Table. Characteristics of hormonal effects
There are several options for classifying hormones. By chemical nature Hormones are divided into three groups: polypeptide and protein, steroid and tyrosine amino acid derivatives.
By functional significance Hormones are also divided into three groups:
- effector, acting directly on target organs;
- tropic, which are produced in the pituitary gland and stimulate the synthesis and release of effector hormones;
- regulating the synthesis of tropic hormones (liberins and statins), which are secreted by neurosecretory cells of the hypothalamus.
Hormones of different chemical natures have common biological properties: long-distance action, high specificity and biological activity.
Steroid hormones and amino acid derivatives are not species specific and have the same effect on animals different types. Protein and peptide hormones are species specific.
Protein-peptide hormones are synthesized in the ribosomes of the endocrine cell. The synthesized hormone is surrounded by membranes and exits as a vesicle to the plasma membrane. As the vesicle moves, the hormone in it “ripens.” After fusion with the plasma membrane, the vesicle ruptures and the hormone is released into the environment(exocytosis). On average, the period from the beginning of hormone synthesis to their appearance at the sites of secretion is 1-3 hours. Protein hormones are highly soluble in the blood and do not require special carriers. They are destroyed in the blood and tissues with the participation of specific enzymes - proteinases. Their half-life in the blood is no more than 10-20 minutes.
Steroid hormones are synthesized from cholesterol. Their half-life is within 0.5-2 hours. There are special carriers for these hormones.
Catecholamines are synthesized from the amino acid tyrosine. Their half-life is very short and does not exceed 1-3 minutes.
Blood, lymph and intercellular fluid transport hormones in free and bound form. 10% of the hormone is transported in free form; bound to blood proteins - 70-80% and adsorbed on shaped elements blood - 5-10% of the hormone.
The activity of bound forms of hormones is very low, since they cannot interact with their specific receptors on cells and tissues. Free hormones are highly active.
Hormones are destroyed under the influence of enzymes in the liver, kidneys, target tissues and the endocrine glands themselves. Hormones are removed from the body through the kidneys, sweat and salivary glands, as well as the gastrointestinal tract.
Regulation of the activity of the endocrine glands
The nervous and humoral systems take part in the regulation of the activity of the endocrine glands.
Humoral regulation- regulation using various classes of physiologically active substances.
Hormonal regulation- part of humoral regulation, including the regulatory effects of classical hormones.
Nervous regulation is carried out mainly through the neurohormones secreted by it. The nerve fibers innervating the glands affect only their blood supply. Therefore, the secretory activity of cells can only change under the influence of certain metabolites and hormones.
Humoral regulation occurs through several mechanisms. Firstly, the concentration of a certain substance, the level of which is regulated by this hormone, can have a direct effect on the cells of the gland. For example, the secretion of the hormone insulin increases when the concentration of glucose in the blood increases. Secondly, the activity of one endocrine gland can be regulated by other endocrine glands.
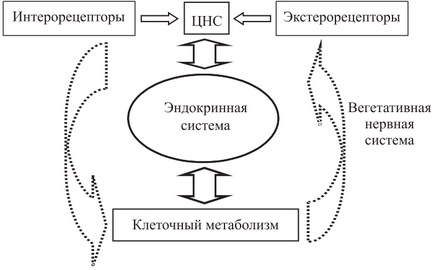
Rice. Unity of nervous and humoral regulation
Due to the fact that the main part of the nervous and humoral regulatory pathways converges at the level of the hypothalamus, a single neuroendocrine regulatory system is formed in the body. And the main connections between the nervous and endocrine regulatory systems are carried out through the interaction of the hypothalamus and pituitary gland. Nerve impulses entering the hypothalamus activate the secretion of releasing factors (liberins and statins). The target organ for liberins and statins is the anterior pituitary gland. Each of the liberins interacts with a certain population of adenohypophysis cells and causes the synthesis of the corresponding hormones in them. Statins have the opposite effect on the pituitary gland, i.e. suppress the synthesis of certain hormones.
Table. Comparative characteristics nervous and hormonal regulation
Note. Both types of regulation are interconnected and influence each other, forming a single coordinated mechanism of neurohumoral regulation with the leading role of the nervous system

Rice. Interaction between the endocrine glands and the nervous system
Interrelations in the endocrine system can also occur according to the “plus or minus interaction” principle. This principle was first proposed by M. Zavadovsky. According to this principle, a gland that produces a hormone in excess has an inhibitory effect on its further release. Conversely, a lack of a certain hormone increases its secretion by the gland. In cybernetics, such a connection is called “negative feedback”. This regulation can be carried out on different levels with inclusion of long or short feedback. Factors that suppress the release of any hormone may be the concentration in the blood of the hormone itself or its metabolic products.
Endocrine glands also interact in a positive way. In this case, one gland stimulates the other and receives activating signals from it. Such “plus-plus interactions” relationships contribute to the optimization of the metabolite and the rapid execution of a vital process. In this case, after achieving the optimal result, the “minus interaction” system is activated to prevent hyperfunction of the glands. Changes in such interconnections of systems constantly occur in the animal body.
Particular physiology of endocrine glands
Hypothalamus
This central structure of the nervous system regulating endocrine functions. located in and includes the preoptic area, the area of the optic chiasm, the infundibulum and the mamillary bodies. In addition, it contains up to 48 paired nuclei.
There are two types of neurosecretory cells in the hypothalamus. The suprachiasmatic and paraventricular nuclei of the hypothalamus contain nerve cells that connect by axons to the posterior lobe of the pituitary gland (neurohypophysis). The cells of these neurons synthesize hormones: vasopressin, or antidiuretic hormone, and oxytocin, which then travel along the axons of these cells to the neurohypophysis, where they accumulate.
Cells of the second type are located in the neurosecretory nuclei of the hypothalamus and have short axons that do not extend beyond the hypothalamus.
In the cells of these nuclei, two types of peptides are synthesized: some stimulate the formation and release of adenohypophysis hormones and are called releasing hormones (or liberins), others inhibit the formation of adenohypophysis hormones and are called statins.
Liberins include: thyreoliberin, somatoliberin, luliberin, prolactoliberin, melanoliberin, corticoliberin, and statins - somatostatin, prolactostatin, melanostatin. Liberins and statins enter by axonal transport into the median eminence of the hypothalamus and are released into the blood of the primary network of capillaries formed by the branches of the superior pituitary artery. Then, with the blood flow, they enter the secondary network of capillaries located in the adenohypophysis and affect its secretory cells. Through the same capillary network, hormones of the adenohypophysis enter the bloodstream and reach the peripheral endocrine glands. This feature of blood circulation in the hypothalamic-pituitary region is called the portal system.
The hypothalamus and pituitary gland unite into a single one, which regulates activity peripheral glands internal secretion.
The secretion of certain hypothalamic hormones is determined by a specific situation, which shapes the nature of direct and indirect influences on the neurosecretory structures of the hypothalamus.
Pituitary
It is located in the fossa of the sella turcica of the main bone and is connected to the base of the brain with the help of a pedicle. consists of three lobes: anterior (adenohypophysis), intermediate and posterior (neurohypophysis).
All hormones of the anterior pituitary gland are protein substances. The production of a number of hormones of the anterior pituitary gland is regulated by liberins and statins.
The adenohypophysis produces six hormones.
Somatotropic hormone(GH,) stimulates protein synthesis in organs and tissues and regulates the growth of young animals. Under its influence, the mobilization of fat from the depot and its use in energy metabolism. If there is a lack of growth hormone in childhood, growth retardation occurs, and the person grows up to be a dwarf, and if it is produced in excess, gigantism develops. If the production of GH increases in adulthood, those parts of the body that are still capable of growing enlarge - fingers and toes, hands, feet, nose and lower jaw. This disease is called acromegaly. The release of somatotropic hormone from the pituitary gland is stimulated by somatoliberin and inhibited by somatostatin.
Prolactin(luteotropic hormone) stimulates the growth of the mammary glands and during lactation increases their secretion of milk. IN normal conditions regulates the growth and development of the corpus luteum and follicles in the ovaries. IN male body affects the formation of androgens and spermiogenesis. Prolactin secretion is stimulated by prolactoliberin, and prolactin secretion is reduced by prolactostatin.
Adrenocorticotropic hormone(ACTH) causes the proliferation of the zona fasciculata and reticularis of the adrenal cortex and enhances the synthesis of their hormones - glucocorticoids and mineralocorticoids. ACTH also activates lipolysis. The release of ACTH from the pituitary gland is stimulated by corticoliberin. ACTH synthesis increases with pain, stressful conditions, physical activity.
Thyroid-stimulating hormone(TSH) stimulates the function of the thyroid gland and activates the synthesis of thyroid hormones. The release of TSH from the pituitary gland is regulated by hypothalamic thyrotropin-releasing hormone, norepinephrine, and estrogens.
Cell stimulating hormone(FSH) stimulates the growth and development of follicles in the ovaries and is involved in spermiogenesis in males. Refers to gonadotropic hormones.
Luteinizing hormone(LH), or lutropin, promotes ovulation of follicles in females, supports the functioning of the corpus luteum and the normal course of pregnancy, and is involved in spermiogenesis in males. It is also a gonadotropic hormone. The formation and release of FSH and LH from the pituitary gland is stimulated by gonadoliberin.
The middle lobe of the pituitary gland produces melanocyte stimulating hormone(MSH), the main function of which is to stimulate the synthesis of the melanin pigment, as well as to regulate the size and number of pigment cells.
Hormones are not synthesized in the posterior lobe of the pituitary gland, but come here from the hypothalamus. Two hormones accumulate in the neurohypophysis: antidiuretic (ADH), or resin flowerpot, And oxytocin.
Influenced ADH diuresis is reduced and drinking behavior is regulated. Vasopressin increases water reabsorption in the distal nephron by increasing the permeability to water of the walls of the distal convoluted tubules and collecting ducts, thereby exerting an antidiuretic effect. By changing the volume of circulating fluid, ADH regulates the osmotic pressure of body fluids. In high concentrations, it causes contraction of arterioles, which leads to an increase in blood pressure.
Oxytocin stimulates the contraction of the smooth muscles of the uterus and regulates the course of labor, and also affects the secretion of milk, enhancing the contractions of myoepithelial cells in the mammary glands. The act of sucking reflexively promotes the release of oxytocin from the neurohypophysis and milk production. In males, it provides a reflex contraction of the vas deferens during ejaculation.
Pineal gland
Prostaglandin E1 and especially prostacyclin: inhibition of platelet adhesion, prevention of the formation of vascular blood clots
Prostaglandin E2: stimulation of platelet adhesion
Increased blood flow to the kidneys, increased urine output and electrolytes. Antagonism with the renal pressor system
Reproductive system
Increased contraction of the uterus during pregnancy. Contraceptive effect. Induction of labor and termination of pregnancy. Increased sperm motility
central nervous system
Irritation of thermoregulatory centers, fever, throbbing headache
This article turned out to be the largest on the blog. It reveals the basic concepts of influence endocrine system and hormones produced by the endocrine glands, on the well-being and state of human health. I propose to understand the issues of endocrine diseases that are unclear to many people and prevent serious disorders in your body.
This publication uses materials from articles posted on the Internet, materials from academic literature, the Guide to Endocrinology, lectures by Professor Park Jae-woo and my personal experience doctor - reflexologist.
Endocrine glands or endocrine glands do not have excretory ducts. They release the products of their vital activity - hormones - into the internal environment of the body: into the blood, lymph, tissue fluid.
Hormones are organic substances of various chemical natures, have:
High biological activity, therefore produced in very small quantities;
The specificity of the action affects organs and tissues located far from the place of hormone production.
Entering the blood, they are distributed throughout the body and carry out humoral regulation of the functions of organs and tissues, stimulate or inhibit their work.
The endocrine glands use hormones to influence metabolic processes, growth, mental, physical, sexual development, the body’s adaptation to changing conditions of the external and internal environment, ensure homeostasis - the constancy of the most important physiological indicators, and also ensure the body’s response to stress.
If the activity of the endocrine glands is disrupted, endocrine diseases occur. Violations may be related to increased function glands, when an increased amount of the hormone is formed and released into the blood, or with reduced function, when a reduced amount of the hormone is formed and released into the blood.
The most important endocrine glands: pituitary gland, thyroid, thymus, pancreas, adrenal glands, gonads, pineal gland. The hypothalamus, the subthalamic region of the diencephalon, also has an endocrine function.
The most important endocrine gland is the pituitary gland or the lower appendage of the brain, its mass is 0.5 g. It produces hormones that stimulate the functions of other endocrine glands. The pituitary gland has three lobes: anterior, middle and posterior. Each produces different hormones.
The anterior lobe of the pituitary gland produces the following hormones.
A. Hormones that stimulate synthesis and secretion:
- thyroid gland – thyrotropins;
- adrenal glands - corticotropins;
- sex glands - gonadotropins;
B. Hormones affecting fat metabolism - lipotropins;
With a lack of hormones of the anterior pituitary gland, increased separation of water from the body with urine, dehydration, lack of skin pigmentation, and obesity occurs. An excess of these hormones increases the activity of all endocrine glands.
B. Growth hormone is somatotropin.
It regulates the growth and development of the body at a young age, as well as protein, fat and carbohydrate metabolism s.
Excessive production of the hormone in childhood and adolescence causes gigantism, and in adults the disease is acromegaly, in which the ears, nose, lips, hands, and feet grow.
Lack of somatotropin in childhood leads to dwarfism. Body proportions and mental development remain normal.
Normally, the production of the hormone somatotropin is promoted by sufficient good dream, especially in childhood. If you want to sleep, sleep. It promotes mental health and beauty. In adults, somatotropin during sleep will help eliminate muscle blocks and relax tense muscles.
Somatotropin is released during deep sleep, so a calm, quiet, comfortable place to sleep is very important.
The middle lobe of the pituitary gland produces a hormone that affects skin pigmentation - melanotropin.
Hormones of the posterior lobe of the pituitary gland increase the reabsorption of water in the kidneys, reduce urination (antidiuretic hormone), and increase the contraction of the smooth muscles of the uterus (oxytocin).
Oxytocin is a pleasure hormone that is produced from pleasant communication.
If a person has little oxytocin, then he has little contact, is irritable, and lacks sensual relationships and tenderness. Oxytocin stimulates the production mother's milk and evokes tenderness in a woman towards her child.
Body hugs, sexual contact, massage, and self-massage promote the production of oxytocin.
The pituitary gland also produces the hormone prolactin. Along with the female sex hormone progesterone, prolactin ensures the growth and development of the mammary glands and their production of milk during the feeding period.
This hormone is called stress. Its content increases with increased physical activity, fatigue, and psychological trauma.
An increase in prolactin levels can cause mastopathy in women, as well as discomfort in the mammary glands in " critical days", may cause infertility. In men there is an excess normal level this hormone causes impotence.
Thyroid located on a person's neck in front of the trachea on top thyroid cartilage. Consists of two lobes connected by an isthmus.
It produces the hormones thyroxine and triiodothyronine, which regulate metabolism and increase the excitability of the nervous system.
With excessive production of thyroid hormones, Graves' disease occurs, metabolism and nervous system excitability increase, goiter and bulging eyes develop.
With a lack of hormones, the disease myxedema develops, metabolism decreases, neuropsychic activity is inhibited, lethargy, drowsiness, apathy develop, swelling of the face and legs, obesity appears, and in adolescence dwarfism and cretinism develop - mental and mental retardation. physical development.
About thyroxine. This is an energy hormone.
Affects a person’s well-being and level of mood. Controls the functioning of vital organs - gall bladder, liver, kidneys.
Physical activity, gymnastics, and breathing exercises, meditation, eating iodine-containing foods: sea fish, seafood - shrimp, mussels, squid, seaweed.
Parathyroid glands. There are four of them. They are located on the posterior surface of the thyroid gland. They produce parathyroid hormone, which regulates the exchange of calcium and phosphorus in the body.
With excess function of the glands, the release of calcium from the bones into the blood and the removal of calcium and phosphates from the body through the kidneys increases. In this case, muscle weakness develops, calcium and phosphorus can be deposited in the form of stones in the kidneys and urinary tract.
In case of defeat parathyroid glands and a decrease in the level of calcium in the blood, the excitability of the nervous system increases, cramps of all muscles appear, and death may occur from paralysis of the respiratory muscles.
Thymus gland (thymus). A small lymphoid organ located behind top part sternum in the mediastinum. Produces the hormones thymosin, thymopoietin and thymalin.
This is an endocrine gland involved in lymphopoiesis - the formation of lymphocytes and immunological defensive reactions, is the central authority cellular immunity, takes part in the regulation of humoral immunity. In childhood, this gland forms immunity, so it is much more active than in adults.
Pancreas located in abdominal cavity below the stomach. In it except for digestive enzymes, The hormones glucagon, insulin and somatostatin are produced.
Glucagon increases blood glucose levels, breaks down glycogen, and releases glucose from the liver. With an excess of glucagon, blood glucose levels increase and fat breakdown occurs. If there is a deficiency, the level of glucose in the blood decreases.
Insulin lowers blood glucose levels and moves glucose into the cell, where it is broken down to produce energy. This supports the vital processes of the cell, glycogen synthesis, and fat deposition.
With insufficient insulin production, type 1 diabetes mellitus occurs, in which glucose levels rise and sugar may appear in the urine. Thirst appears copious discharge urine, skin itching.
As the disease progresses, pain appears in the limbs, vision is impaired due to damage to the retina, appetite decreases, and kidney damage develops. The most severe complication diabetes mellitus- diabetic coma.
With an excess of insulin, a hypoglycemic state may occur, accompanied by convulsions, loss of consciousness, and a hypoglycemic coma may develop.
Somatostatin – inhibits the formation and release of glucagon.
Adrenal glands. They are located in the upper part of the kidneys, above them. They have two layers: outer - cortical and inner - medulla.
Hormones of the cortical layer - corticoids (glucocorticoids, mineralocorticoids, sex hormones, aldosterone) regulate the exchange of mineral and organic substances, the release of sex hormones, and suppress allergic and inflammatory processes.
Excessive function of these hormones in youth leads to early puberty with rapid cessation of growth, and in adults – to disruption of the manifestation of secondary sexual characteristics
.
With a lack of these hormones, bronze disease (Addisson's disease) occurs, manifested by a bronze skin tone reminiscent of a tan, weakness, weight loss, decreased appetite, decreased blood pressure, dizziness, fainting, and abdominal pain. Removal of the adrenal cortex or hemorrhage into these organs can lead to death due to loss large quantity fluids – dehydration of the body.
The adrenal hormones cortisol and aldosterone play a particularly important role.
Cortisol is produced in large quantities during stress. It triggers immune defense processes: protects against stress, activates the activity of the heart and brain.
At elevated level Cortisol causes increased fat deposition on the abdomen, back, and back of the neck.
A decrease in cortisol below normal impairs immunity, a person begins to get sick often, and acute adrenal insufficiency may develop.
At the same time, blood pressure sharply decreases, sweating appears, severe weakness, nausea, vomiting, diarrhea, arrhythmia develops, urine output sharply decreases, consciousness is impaired, hallucinations, fainting, and coma occur. In this case, emergency hospitalization is necessary.
Aldosterone regulates water - salt metabolism, sodium and potassium content in the blood, supports enough level glucose in the blood, formation and deposition of glycogen in the liver and muscles. The last two functions of the adrenal glands are performed jointly with pancreatic hormones.
Hormones of the adrenal medulla - adrenaline and norepinephrine, regulate the functioning of the heart, blood vessels, digestion, and break down glycogen. They are released during strong stressful emotions - anger, fear, pain, danger. Provides the body's response to stress.
When these hormones enter the blood, a rapid heartbeat occurs, a narrowing of blood vessels except those of the heart and brain, an increase in blood pressure, increased breakdown of glycogen in the liver and muscles to glucose, inhibition of intestinal motility, relaxation of the bronchial muscles, increased excitability of the receptors of the retina, auditory and vestibular apparatus. The body's strength is mobilized to endure stressful situations.
Adrenaline is the hormone of fear, danger and aggression. In these states Under the influence of adrenaline, a person is at the maximum of physical and mental abilities. An excess of adrenaline dulls the feeling of fear, a person becomes dangerous and aggressive.
People who have poor adrenaline production often give in to life's difficulties.
Adrenaline levels are increased by physical activity, sex, and black tea.
Calming infusions reduce adrenaline and aggression medicinal herbs– motherwort herb, root and rhizome of valerian.
Norepinephrine is a hormone of relief and happiness. It neutralizes the fear hormone adrenaline. Norepinephrine provides relief, relaxes, normalizes psychological condition after stress, when you want to breathe a sigh of relief “the worst is over.”
The production of norepinephrine is stimulated by the sound of the surf, contemplation of pictures of nature, the sea, distant mountains, beautiful landscapes, and listening to pleasant relaxing music.
Sex glands (gonads).
Testicles in men, allocate spermatozoa into the external environment, and sperm into the internal environment androgen hormone - testosterone.
It is necessary for the formation of the reproductive system in the embryo male type, is responsible for the development of primary and secondary sexual characteristics, stimulates the development of the gonads, the maturation of germ cells.
It also stimulates protein synthesis, and this accelerates the processes of growth, physical development, enlargement muscle mass. This is the most male hormone. It incites a man to aggression, forces him to hunt, kill prey, provide food, protect his family and home.
Thanks to testosterone, men grow a beard, their voice becomes deep, a bald spot appears on their head, and the ability to navigate in space develops. A man who has a deeper voice tends to be more sexually active.
In men who drink alcohol excessively and smokers, testosterone levels decrease. A natural decline in testosterone levels in men occurs after 50 - 60 years, they become less aggressive, willingly babysit children and do housework.
Currently, many and even young men have low testosterone levels. This is due to the wrong lifestyle of men. Alcohol abuse, smoking, unbalanced diet, insufficient sleep, and insufficient physical activity create health problems and reduce testosterone levels.
Wherein:
- decreases sexual function And sexual desire,
- muscle mass decreases,
- secondary sexual characteristics disappear: the low voice disappears, the man’s figure acquires rounded shapes,
- vitality decreases,
- fatigue, irritability appear,
- depression develops
- decreased ability to concentrate,
- memory and ability to memorize deteriorate,
- slowing down metabolic processes and deposition of adipose tissue.
Testosterone levels can be increased naturally.
1.Due to nutrition.
Minerals. The body must enter zinc in sufficient quantities, which is needed for the synthesis of testosterone.
Zinc is found in seafood (squid, mussels, shrimp), fish (salmon, trout, saury), nuts ( Walnut, peanuts, pistachios, almonds), pumpkin and sunflower seeds. Other minerals involved in testosterone synthesis: selenium, magnesium, calcium.
Vitamins. Important role have a role in testosterone synthesis vitamins C, E, F and B vitamins. They are found in citrus fruits, black currant, rosehip, fish oil, avocado, nuts.
Food must contain proteins, fats, and carbohydrates as the basis of human nutrition. The diet of men should include lean meat and fats as a source of cholesterol, from which testosterone is synthesized.
2. To maintain normal testosterone levels, a man needs moderate physical activity– working out in the gym with weights, working in a summer cottage.
3. Sleep at least 7 - 8 hours in complete silence and darkness. Sex hormones are synthesized during deep sleep. Constant lack of sleep reduces testosterone levels in the blood.
Ovaries in women, secrete into the external environment of the egg, and hormones - estrogens and progestins - into the internal environment.
Estrogens include estradiol. This is the most female hormone.
It determines the regularity of the menstrual cycle, in girls it causes the formation of secondary sexual characteristics - enlargement of the mammary glands, growth of hair on the pubis and vulva corresponding to the female type. armpits, development of a wide female pelvis.
Estrogen prepares the girl for sex life and motherhood.
Estrogen allows adult women to maintain youth, beauty, good condition skin and a positive attitude towards life.
This hormone creates a woman’s desire to nurse children and protect “her nest”.
In adolescents - a decrease in the size of the uterus and mammary glands, absence of menstruation.
In women of childbearing age: insomnia, mood swings, irregular periods, decreased libido, pain in the lower abdomen during menstruation, memory loss, decreased performance, changes in the skin - stretch marks, inflammation, decreased elasticity - hardening. Consequence low level estrogen may cause infertility.
Reasons for decreased estrogen levels: lack of vitamins, poor nutrition, sudden weight loss, menopause, long-term use oral contraceptives.
The decision to increase estrogen levels must be made by a gynecologist.
How to increase estrogen levels?
In addition to the reception hormonal drugs and vitamin E, which are prescribed by a gynecologist, estrogen levels, if necessary, can be increased with certain foods that are included in the diet.
These include:
- cereals and legumes - soybeans, beans, peas, corn, barley, rye, millet;
- fats of animal origin, which are found in dairy products, meat, hard cheese, fish oil;
- vegetables – carrots, tomatoes, eggplants, cauliflower and Brussels sprouts;
- fruits – apples, dates, pomegranates;
- green tea;
- sage decoction.
It should be recalled that excess estrogen in a woman’s body can lead to headaches, nausea, and insomnia, so women should discuss estrogen treatment with their doctor.
Progestins include progesterone, a hormone that promotes the timely onset and normal development of pregnancy.
It is necessary for the attachment of a fertilized egg - an embryo - to the wall of the uterus. During pregnancy, it inhibits the maturation and ovulation of other follicles.
Progesterone is produced by the corpus luteum, placenta and adrenal glands. This is the hormone of parental instinct. Under its influence, a woman physically prepares for childbirth and experiences psychological changes. Progesterone prepares a woman's mammary glands to produce milk when the baby is born.
A woman's blood progesterone levels increase when she sees small children. This is a strong reaction. Progesterone is actively released even if a woman sees something like a baby soft toy(doll, teddy bear).
Lack of progesterone can disrupt women's reproductive system and promote development gynecological diseases(endometriosis, uterine fibroids, mastopathy).
The main symptoms of progesterone deficiency: irritability and Bad mood, headaches, breast swelling, swelling in the legs and face, irregular menstrual cycle.
Reasons for decreased progesterone levels: stress, poor nutrition, alcohol abuse and smoking, unfavorable environmental conditions.
For natural increase progesterone levels, you should take B vitamins and vitamin E, and the microelement zinc.
You should include nuts in your diet beef liver, rabbit meat, pumpkin and sunflower seeds, beans and wheat bran, soybeans, meat and fish products, eggs, cheese, red and black caviar.
During menopause, a woman's estrogen level decreases and the level of testosterone, which is produced by the adrenal glands in women, increases. Her behavior changes, she becomes more independent, decisive, shows organizational skills and a tendency to entrepreneurial activity. There may be growth of facial hair, a tendency to stress, and the likelihood of developing a stroke.
During the period from the 21st to the 28th day monthly cycle level female hormones blood levels drop sharply, and “critical days” begin.
The following symptoms develop: irritability, increased fatigue, aggression, tearfulness, sleep disturbance, headaches, and depression. Can appear acne, pain in the lower abdomen, “hardening” of the mammary glands, swelling in the legs and face, constipation, increased blood pressure. This is due to excess estrogen and lack of progesterone.
The pineal gland is a gland connected to the thalamus. Produces the hormones serotonin and melatonin. They regulate puberty and sleep duration.
Excess of them leads to premature puberty.
The lack of these hormones in youth leads to underdevelopment of the sex glands and secondary sexual characteristics.
Serotonin is the hormone of happiness. It improves mood, reduces stress, and causes a feeling of satisfaction and happiness. This is not just a hormone, it is a neurotransmitter - a transmitter of impulses between nerve cells of the human brain.
Improves under the influence of serotonin cognitive activity person. It has a positive effect on motor activity and muscle tone, creates a feeling of uplifting mood. In combination with other hormones, serotonin allows a person to experience the full range of emotions from satisfaction to happiness and euphoria.
A lack of serotonin in the body causes decreased mood and depression.
In addition to mood, serotonin is responsible for self-control or emotional stability. It controls sensitivity to stress, that is, to the hormones adrenaline and norepinephrine.
In people with reduced level serotonin, the slightest negative reasons cause a strong stress reaction.
People with high level serotonin dominate in society.
To produce serotonin in the body you need:
- ensure the supply of the amino acid tryptophan, which is necessary for the synthesis of serotonin, with food;
- take carbohydrate foods, chocolate, cake, banana, which will increase the level of tryptophan in the blood and, accordingly, serotonin.
It is better to increase serotonin levels with moderate physical activity in the gym, use your favorite perfume, or take a warm bath with your favorite scent.
Melatonin is a sleep hormone produced in the blood in dark time day, regulates the sleep cycle, body biorhythms in the dark, increases appetite, promotes fat deposition.
Endorphin is a hormone of joy, a natural drug, similar in action to serotonin, the main substance that affects the body’s pain-relieving system. Reduces pain and brings a person to euphoria, affects mood, creating positive emotions.
Endorphin is produced in brain cells from betalipotropin, which is secreted by the pituitary gland in stressful situations, fights. At the same time, the pain from the blows is felt less.
Endorphin also:
- calms down,
- increases immunity,
- accelerates the process of tissue and bone restoration in case of fractures,
- increases blood flow to the brain and heart,
- restores blood pressure after stress,
- restores appetite,
- improves the functioning of the digestive system,
- promotes memorization of information received when reading books, watching TV shows, listening to lectures, talking with interlocutors.
Ways to increase endorphins:
- sports involving heavy loads (boxing, wrestling, barbell);
- creativity: painting pictures, composing music, knitting, weaving, wood carving, observing the creativity of others, visiting theaters, museums, art galleries;
- ultraviolet irradiation under the sun;
- laughter.
The production of endorphins is facilitated by power, fame, and the completion of a given task: writing an article, cooking, preparing firewood, etc. Any completed task or achievement of a goal increases endorphin in the body.
Sex promotes the production of endorphin, the hormone of joy and happiness.. Sex, like intense physical activity, improves blood supply to the body's organs.
With regular sexual activity, the body produces adrenaline and cortisol, which stimulate brain function and prevent migraines. Sex increases the ability to concentrate, stimulates attention, creative thinking, and prolongs life.
Dopamine is both a neurotransmitter and a hormone. Produced in brain cells, as well as in the adrenal medulla and other organs, such as the kidneys.
Dopamine is a biochemical precursor of norepinephrine and adrenaline. This is the “flight” hormone. Provides Good work all muscles, easy gait, feeling of lightness and speed. If there is not enough dopamine in the body, the body becomes heavy and the legs move poorly.
Dopamine also:
- stimulates thinking,
- reduces the sensation of pain,
- gives a feeling of flight and bliss,
- influences the processes of motivation and learning,
- causes a feeling of pleasure and satisfaction.
Dopamine is produced during what a person perceives as a positive experience, eating tasty food, during sex, and pleasant bodily sensations. Dancing stimulates the production of dopamine.
The functioning of the endocrine glands, which form the endocrine system, is carried out in interaction with each other and with the nervous system.
All information from the external and internal environment of the body enters the cortex cerebral hemispheres and other parts of the brain where it is processed and analyzed. From them information signals are transmitted to hypothalamus– subtubercular region of the diencephalon.
The hypothalamus produces regulatory hormones that enter the pituitary gland and through it exert their regulating effect on the work of the endocrine glands.
Thus, the hypothalamus is the “supreme commander” in the endocrine system and performs coordinating and regulatory functions.
A review of the endocrine system has been completed, the main hormones and their effect on humans are reflected, signs of disorders in the endocrine system are indicated, and the main symptoms indicating certain endocrine diseases are given.
If you have discovered these signs and symptoms, then you should visit a therapist and endocrinologist, undergo an appropriate examination (blood test for the content of a particular hormone, ultrasound, computer examination of the problem gland) and treatment with the drugs prescribed by the attending physician.
Is it possible for a person himself in everyday life at home to influence the endocrine system to optimize its work and on individual endocrine glands in case of violations of their function?
Yes, you can. To do this, you can use the capabilities of reflexology.
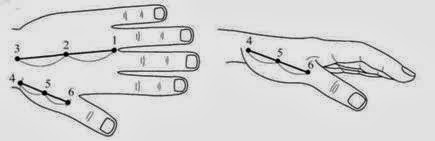
There are special energy points on the hands - basic points (see pictures), which should be warmed up with lighted wormwood sticks using up and down pecking movements.
Energy points on the hand.

 To warm up the points, you can use a high-grade, well-dried cigarette, the end of which is set on fire and the points are warmed up with pecking movements “up and down”, without touching the skin. You should not smoke in this case, as it is very harmful.
To warm up the points, you can use a high-grade, well-dried cigarette, the end of which is set on fire and the points are warmed up with pecking movements “up and down”, without touching the skin. You should not smoke in this case, as it is very harmful.
Basic points can be stimulated by seeds hot pepper, which are glued with a patch to the base points and remain there until a feeling of warmth and redness of the skin appears.
Health, immunity and life expectancy largely depend on the state of the body's endocrine system. In order for the endocrine glands to work effectively, they should also be influenced by reflexology techniques.
You should find the points corresponding to the endocrine glands (see figure), massage them thoroughly, warm them using the above technique and place buckwheat, rose hip, and sea buckthorn seeds on them.
For those who suffer from arterial hypertension and cardiovascular vascular diseases, impact on the points of the endocrine glands should not be carried out, as blood pressure may increase and cardiac disease may develop attack.
1. The physiological role of the endocrine glands. Characteristics of the action of hormones.
Endocrine glands are specialized organs that have a glandular structure and secrete their secretions into the blood. They have no excretory ducts. These glands include: pituitary gland, thyroid gland, parathyroid gland, adrenal glands, ovaries, testes, thymus gland, pancreas, pineal gland, APUD system (amine precursor uptake system and their decarboxylation), as well as the heart - produces atrial sodium -diuretic factor, kidneys - produce erythropoietin, renin, calcitriol, liver - produce somatomedin, skin - produce calciferol (vitamin D 3), gastrointestinal tract - produce gastrin, secretin, cholicystokinin, VIP (vasointestinal peptide), GIP (gastroinhibitory peptide).
Hormones perform the following functions:
Participate in maintaining homeostasis of the internal environment, controlling glucose levels, extracellular fluid volume, blood pressure, and electrolyte balance.
Provide physical, sexual, mental development. They are also responsible for the reproductive cycle ( menstrual cycle, ovulation, spermatogenesis, pregnancy, lactation).
Monitor education and use nutrients and energy resources in the body
Hormones provide adaptation processes physiological systems to the action of stimuli from the external and internal environment and participate in behavioral reactions (need for water, food, sexual behavior)
They are intermediaries in the regulation of functions.
The endocrine glands create one of two systems for regulating functions. Hormones differ from neurotransmitters because they change chemical reactions in the cells they act on. Neurotransmitters cause an electrical reaction.
The term “hormone” comes from the Greek word HORMAE - “I excite, motivate.”
Classification of hormones.
By chemical structure:
1. Steroid hormones are derivatives of cholesterol (hormones of the adrenal cortex, gonads).
2. Polypeptide and protein hormones (anterior pituitary gland, insulin).
3. Tyrosine amino acid derivatives (adrenaline, norepinephrine, thyroxine, triiodothyronine).
By functional value:
1. Tropic hormones (activate the activity of other endocrine glands; these are hormones of the anterior pituitary gland)
2. Effector hormones (act directly on metabolic processes in target cells)
3. Neurohormones (released in the hypothalamus - liberins (activating) and statins (inhibiting)).
Properties of hormones.
Distant nature of action (for example, pituitary hormones affect the adrenal glands),
Strict specificity of hormones (the absence of hormones leads to loss of a certain function, and this process can only be prevented by the introduction of the necessary hormone),
They have high biological activity (formed in low concentrations in liquid liquids.),
Hormones do not have ordinary specificity,
They have a short half-life (they are quickly destroyed by tissues, but have a long-lasting hormonal effect).
2. Mechanisms of hormonal regulation of physiological functions. Its features compared to nervous regulation. Systems of direct and reverse (positive and negative) connections. Methods for studying the endocrine system.
Internal secretion (incretion) is the secretion of specialized biologically active substances - hormones- into the internal environment of the body (blood or lymph). Term "hormone" was first applied to secretin (the gut hormone) by Starling and Baylis in 1902. Hormones differ from other biologically active substances, for example, metabolites and mediators, in that they, firstly, are formed by highly specialized endocrine cells, and secondly, in that they influence tissues distant from the gland through the internal environment, i.e. have a distant effect.
The most ancient form of regulation is humoral-metabolic(diffusion of active substances to neighboring cells). She in various forms occurs in all animals, especially clearly manifested in the embryonic period. The nervous system, as it developed, subordinated itself to humoral-metabolic regulation.
True endocrine glands appeared late, but early stages there is evolution neurosecretion. Neurosecrets are not mediators. Mediators are simpler compounds, work locally in the synapse area and are quickly destroyed, while neurosecrets are protein substances, break down more slowly and work over a long distance.
With the advent circulatory system neurosecrets began to be released into her cavity. Then special formations arose to accumulate and change these secretions (in ringed fish), then their appearance became more complex and the epithelial cells themselves began to release their secretions into the blood.
Endocrine organs have the most different origins. Some of them arose from the sense organs (the pineal gland - from the third eye). Other endocrine glands were formed from the exocrine glands (thyroid). Branchiogenic glands were formed from the remains of provisional organs (thymus, parathyroid glands). Steroid glands originate from the mesoderm, from the walls of the coelom. Sex hormones are secreted by the walls of glands containing germ cells. thus different endocrine organs have different origins, but they all arose as additional method regulation. There is a unified neurohumoral regulation in which the nervous system plays a leading role.
Why was such an addition to nervous regulation formed? Neural connection- fast, accurate, locally addressed. Hormones act more widely, more slowly, longer. They provide a long-term reaction without the participation of the nervous system, without constant impulses, which is uneconomical. Hormones have a long aftereffect. When required fast reaction- the nervous system works. When a slower and more persistent reaction to slow and long-term changes in the environment is required, hormones work (spring, autumn, etc.), providing all adaptive changes in the body, including sexual behavior. In insects, hormones completely ensure all metamorphosis.
The nervous system acts on the glands in the following ways:
1. Through neurosecretory fibers of the autonomic nervous system;
2.Through neurosecrets - the formation of the so-called. releasing or inhibiting factors;
3. The nervous system can change the sensitivity of tissues to hormones.
Hormones also affect the nervous system. There are receptors that respond to ACTH, to estrogens (in the uterus), hormones affect the GNI (sexual), the activity of the reticular formation and hypothalamus, etc. Hormones influence behavior, motivation and reflexes, and are involved in stress reactions.
There are reflexes in which the hormonal part is included as a link. For example: cold - receptor - central nervous system - hypothalamus - releasing factor - secretion of thyroid-stimulating hormone - thyroxine - increase in cellular metabolism - increase in body temperature.
Methods for studying the endocrine glands.
1. Removal of the gland - extirpation.
2. Gland transplantation, injection of extract.
3. Chemical blockade of gland functions.
4. Determination of hormones in liquid media.
5. Method of radioactive isotopes.
3. Mechanisms of interaction of hormones with cells. Concept of target cells. Types of hormone reception by target cells. The concept of membrane and cytosolic receptors.
Peptide (protein) hormones are produced in the form of prohormones (their activation occurs during hydrolytic cleavage), water-soluble hormones accumulate in cells in the form of granules, fat-soluble (steroids) are released as they are formed.
For hormones in the blood, there are carrier proteins - these are transport proteins that can bind hormones. In this case, no chemical reactions occur. Some hormones can be transported in dissolved form. Hormones are delivered to all tissues, but only cells that have receptors for the action of the hormone respond to the action of hormones. Cells that carry receptors are called target cells. Target cells are divided into: hormone-dependent and
hormone sensitive.
The difference between these two groups is that hormone-dependent cells can only develop in the presence of this hormone. (So, for example, germ cells can develop only in the presence of sex hormones), and hormone-sensitive cells can develop without hormones, but they are able to perceive the action of these hormones. (So, for example, cells of the nervous system develop without the influence of sex hormones, but perceive their action).
Each target cell has a specific receptor for the action of the hormone, and some of the receptors are located in the membrane. This receptor is stereospecific. In other cells, receptors are located in the cytoplasm - these are cytosolic receptors that react together with the hormone that penetrates into the cell.
Consequently, receptors are divided into membrane and cytosolic. In order for a cell to respond to the action of a hormone, the formation of secondary messengers to the action of hormones is necessary. This is typical for hormones with a membrane type of reception.
4. Systems of secondary messengers of the action of peptide hormones and catecholamines.
The systems of secondary messengers of hormone action are:
1. Adenylate cyclase and cyclic AMP,
2. Guanylate cyclase and cyclic GMP,
3. Phospholipase C:
Diacylglycerol (DAG),
Inositol tri-phosphate (IF3),
4. Ionized Ca - calmodulin
Heterotromic protein G protein.
This protein forms loops in the membrane and has 7 segments. They are compared to serpentine ribbons. It has protruding (outer) and inner parts. The hormone is attached to the outer part, and on inner surface There are 3 subunits - alpha, beta and gamma. In its inactive state, this protein has guanosine diphosphate. But upon activation, guanosine diphosphate changes to guanosine triphosphate. A change in the activity of the G protein leads either to a change in the ionic permeability of the membrane, or to the activation of the enzyme system in the cell (adenylate cyclase, guanylate cyclase, phospholipase C). This causes the formation of specific proteins, protein kinase is activated (necessary for phosphorylation processes).
G proteins can be activating (Gs) and inhibitory, or in other words, inhibitory (Gi).
The destruction of cyclic AMP occurs under the action of the enzyme phosphodiesterase. Cyclic GMF has the opposite effect. When phospholipase C is activated, substances are formed that promote the accumulation of ionized calcium inside the cell. Calcium activates protein cinases and promotes muscle contraction. Diacylglycerol promotes the conversion of membrane phospholipids into arachidonic acid, which is the source of the formation of prostaglandins and leukotrienes.
The hormone receptor complex penetrates the nucleus and acts on DNA, which changes transcription processes and produces mRNA, which leaves the nucleus and goes to the ribosomes.
Therefore, hormones can have:
1. Kinetic or starting action,
2. Metabolic action,
3. Morphogenetic effect (tissue differentiation, growth, metamorphosis),
4. Corrective action (corrective, adapting).
Mechanisms of action of hormones in cells:
Changes in cell membrane permeability,
Activation or inhibition of enzyme systems,
Impact on genetic information.
Regulation is based on close cooperation endocrine and nervous system. Excitation processes in the nervous system can activate or inhibit the activity of the endocrine glands. (Consider, for example, the process of ovulation in a rabbit. Ovulation in a rabbit occurs only after mating, which stimulates the release of gonadotropic hormone from the pituitary gland. The latter causes the ovulation process).
After suffering mental trauma, thyrotoxicosis may occur. The nervous system controls the release of pituitary hormones (neurohormones), and the pituitary gland influences the activity of other glands.
Feedback mechanisms exist. The accumulation of a hormone in the body leads to inhibition of the production of this hormone by the corresponding gland, and the deficiency will be a mechanism for stimulating the formation of the hormone.
There is a mechanism of self-regulation. (For example, the level of glucose in the blood determines the production of insulin and (or) glucagon; if the sugar level increases, insulin is produced, and if it decreases, glucagon is produced. Na deficiency stimulates the production of aldosterone).
6. Adenohypophysis, its connection with the hypothalamus. The nature of the action of hormones of the anterior pituitary gland. Hypo- and hypersecretion of adenohypophysis hormones. Age-related changes formation of anterior lobe hormones.
The cells of the adenohypophysis (see their structure and composition in the histology course) produce the following hormones: somatotropin (growth hormone), prolactin, thyrotropin (thyroid-stimulating hormone), follicle-stimulating hormone, luteinizing hormone, corticotropin (ACTH), melanotropin, beta-endorphin, diabetogenic peptide, exophthalmic factor and ovarian growth hormone. Let's take a closer look at the effects of some of them.
Corticotropin . (adrenocorticotropic hormone - ACTH) is secreted by the adenohypophysis in continuously pulsating bursts that have a clear daily rhythm. The secretion of corticotropin is regulated by direct and feedback connections. The direct connection is represented by the hypothalamic peptide - corticoliberin, which enhances the synthesis and secretion of corticotropin. Feedback is triggered by the content of cortisol in the blood (a hormone of the adrenal cortex) and is closed both at the level of the hypothalamus and the adenohypophysis, and an increase in the concentration of cortisol inhibits the secretion of corticotropin and corticotropin.
Corticotropin has two types of action - adrenal and extra-adrenal. The adrenal action is the main one and consists of stimulating the secretion of glucocorticoids, and to a much lesser extent, mineralocorticoids and androgens. The hormone enhances the synthesis of hormones in the adrenal cortex - steroidogenesis and protein synthesis, leading to hypertrophy and hyperplasia of the adrenal cortex. The extra-adrenal effect consists of lipolysis of adipose tissue, increased insulin secretion, hypoglycemia, increased melanin deposition with hyperpigmentation.
Excess corticotropin is accompanied by the development of hypercortisolism with a predominant increase in cortisol secretion and is called “Itsenko-Cushing’s disease.” The main manifestations are typical for excess glucocorticoids: obesity and other metabolic changes, a decrease in the effectiveness of immune mechanisms, development arterial hypertension and the possibility of diabetes. Corticotropin deficiency causes insufficiency of glucocorticoid function of the adrenal glands with pronounced metabolic changes, as well as a decrease in the body's resistance to unfavorable environmental conditions.
Somatotropin . . Growth hormone has a wide range of metabolic effects that provide morphogenetic effects. The hormone affects protein metabolism, enhancing anabolic processes. It stimulates the supply of amino acids into cells, protein synthesis by accelerating translation and activating RNA synthesis, increases cell division and tissue growth, and inhibits proteolytic enzymes. Stimulates the incorporation of sulfate into cartilage, thymidine into DNA, proline into collagen, uridine into RNA. The hormone causes a positive nitrogen balance. Stimulates the growth of epiphyseal cartilage and their replacement with bone tissue by activating alkaline phosphatase.
The effect on carbohydrate metabolism is twofold. On the one hand, somatotropin increases insulin production both due to a direct effect on beta cells and due to the hormone-induced hyperglycemia caused by the breakdown of glycogen in the liver and muscles. Somatotropin activates liver insulinase, an enzyme that destroys insulin. On the other hand, somatotropin has a contrainsular effect, inhibiting the utilization of glucose in tissues. This combination of effects, in the presence of a predisposition in conditions of excessive secretion, can cause diabetes mellitus, called pituitary in origin.
The effect on fat metabolism is to stimulate lipolysis of adipose tissue and the lipolytic effect of catecholamines, increasing the level of free fatty acids in blood; due to their excessive intake into the liver and oxidation, the formation of ketone bodies increases. These effects of somatotropin are also classified as diabetogenic.
If an excess of the hormone occurs in early age, gigantism is formed with proportional development of the limbs and torso. An excess of the hormone in adolescence and adulthood causes increased growth of the epiphyseal areas of skeletal bones, areas with incomplete ossification, which is called acromegaly. . Internal organs also increase in size - splanchomegaly.
With congenital deficiency of the hormone, dwarfism is formed, called “pituitary dwarfism.” After the publication of J. Swift's novel about Gulliver, such people are called colloquial speech Lilliputians. In other cases, acquired hormone deficiency causes mild growth retardation.
Prolactin . The secretion of prolactin is regulated by hypothalamic peptides - the inhibitor prolactinostatin and the stimulator prolactoliberin. The production of hypothalamic neuropeptides is under dopaminergic control. The level of estrogen and glucocorticoids in the blood affects the amount of prolactin secretion
and thyroid hormones.
Prolactin specifically stimulates mammary gland development and lactation, but not its secretion, which is stimulated by oxytocin.
In addition to the mammary glands, prolactin affects the sex glands, helping to maintain the secretory activity of the corpus luteum and the formation of progesterone. Prolactin is a regulator of water-salt metabolism, reducing the excretion of water and electrolytes, potentiates the effects of vasopressin and aldosterone, stimulates growth internal organs, erythropoiesis, contributes to the manifestation of the maternal instinct. In addition to enhancing protein synthesis, it increases the formation of fat from carbohydrates, contributing to postpartum obesity.
Melanotropin . . It is formed in the cells of the intermediate lobe of the pituitary gland. Melanotropin production is regulated by hypothalamic melanoliberin. The main effect of the hormone is on the melanocytes of the skin, where it causes depression of pigment in the processes, an increase in free pigment in the epidermis surrounding the melanocytes, and an increase in melanin synthesis. Increases pigmentation of skin and hair.
7. Neurohypophysis, its connection with the hypothalamus. Effects of posterior pituitary hormones (oxygocin, ADH). The role of ADH in the regulation of fluid volume in the body. Diabetes insipidus.
Vasopressin . . It is formed in the cells of the supraoptic and paraventricular nuclei of the hypothalamus and accumulates in the neurohypophysis. The main stimuli that regulate the synthesis of vasopressin in the hypothalamus and its secretion into the blood by the pituitary gland can generally be called osmotic. They are represented by: a) increase osmotic pressure blood plasma and stimulation of vascular osmoreceptors and osmoreceptor neurons of the hypothalamus; b) an increase in sodium content in the blood and stimulation of hypothalamic neurons that act as sodium receptors; c) a decrease in the central volume of circulating blood and blood pressure, perceived by volume receptors of the heart and mechanoreceptors of blood vessels;
d) emotional-painful stress and physical activity; e) activation of the renin-angiotensin system and the effect of angiotensin stimulating neurosecretory neurons.
The effects of vasopressin are realized due to the binding of the hormone in tissues to two types of receptors. Binding to Y1-type receptors, predominantly localized in the wall of blood vessels, through the second messengers inositol triphosphate and calcium causes vascular spasm, which contributes to the name of the hormone - “vasopressin”. Binding to Y2-type receptors in the distal parts of the nephron through the secondary messenger c-AMP ensures an increase in the permeability of the nephron collecting ducts to water, its reabsorption and urine concentration, which corresponds to the second name of vasopressin - “antidiuretic hormone, ADH”.
In addition to the effect on the kidney and blood vessels, vasopressin is one of the important brain neuropeptides involved in the formation of thirst and drinking behavior, memory mechanisms, and regulation of the secretion of adenopituitary hormones.
Lack or even complete absence Vasopressin secretion manifests itself in the form of a sharp increase in diuresis with the release of large amounts of hypotonic urine. This syndrome is called " diabetes insipidus", it can be congenital or acquired. Excess vasopressin syndrome (Parhon syndrome) manifests itself
in excessive fluid retention in the body.
Oxytocin . The synthesis of oxytocin in the paraventricular nuclei of the hypothalamus and its release into the blood from the neurohypophysis is stimulated by a reflex pathway when irritating the stretch receptors of the cervix and the receptors of the mammary glands. Estrogens increase the secretion of oxytocin.
Oxytocin causes the following effects: a) stimulates contraction of the smooth muscles of the uterus, promoting childbirth; b) causes contraction of smooth muscle cells of the excretory ducts of the lactating mammary gland, ensuring the release of milk; c) has a diuretic and natriuretic effect under certain conditions; d) participates in organizing drinking and eating behavior; d) is additional factor regulation of the secretion of adenopituitary hormones.
8. Adrenal cortex. Hormones of the adrenal cortex and their function. Regulation of corticosteroid secretion. Hypo- and hyperfunction of the adrenal cortex.
Mineralocorticoids are secreted in the zona glomerulosa of the adrenal cortex. The main mineralocorticoid is aldosterone .. This hormone is involved in the regulation of the exchange of salts and water between internal and external environment, predominantly affecting the tubular apparatus of the kidneys, as well as the sweat and salivary glands, and the intestinal mucosa. Acting on the cell membranes of the vascular network and tissues, the hormone also provides regulation of the exchange of sodium, potassium and water between the extracellular and intracellular environment.
The main effects of aldosterone in the kidneys are increased sodium reabsorption in the distal tubules with its retention in the body and increased urinary potassium excretion with a decrease in the cation content in the body. Under the influence of aldosterone, the body retains chlorides, water, and increases the excretion of hydrogen ions, ammonium, calcium and magnesium. The volume of circulating blood increases, a shift in acid-base balance towards alkalosis is formed. Aldosterone can have a glucocorticoid effect, but it is 3 times weaker than cortisol and is not manifested under physiological conditions.
Mineralocorticoids are vital hormones, since the death of the body after removal of the adrenal glands can be prevented by introducing hormones from the outside. Mineralocorticoids increase inflammation, which is why they are sometimes called anti-inflammatory hormones.
The main regulator of the formation and secretion of aldosterone is angiotensin II, which made it possible to consider aldosterone part renin-angiotensin-aldosterone system (RAAS), providing regulation of water-salt and hemodynamic homeostasis. The feedback link in the regulation of aldosterone secretion is realized by changing the level of potassium and sodium in the blood, as well as the volume of blood and extracellular fluid, and the sodium content in the urine of the distal tubules.
Excessive production of aldosterone - aldosteronism - can be primary or secondary. In primary aldosteronism, the adrenal gland, due to hyperplasia or tumor of the zona glomerulosa (Cohn syndrome), produces increased quantities hormone, which leads to sodium and water retention in the body, edema and arterial hypertension, loss of potassium and hydrogen ions through the kidneys, alkalosis and shifts in the excitability of the myocardium and nervous system. Secondary aldosteronism is the result of excess production of angiotensin II and increased stimulation of the adrenal glands.
Aldosterone deficiency due to adrenal damage pathological process It is rarely isolated and is often combined with a deficiency of other cortical hormones. Leading violations are noted from the outside cardiovascular and nervous systems, which is associated with inhibition of excitability,
a decrease in BCC and changes in electrolyte balance.
Glucocorticoids (cortisol and corticosterone ) influence all types of exchange.
Hormones have mainly catabolic and antianabolic effects on protein metabolism and cause a negative nitrogen balance. protein breakdown occurs in muscle, connective bone tissue, the level of albumin in the blood will drop. The permeability of cell membranes to amino acids decreases.
The effects of cortisol on fat metabolism are due to a combination of direct and indirect effects. The synthesis of fat from carbohydrates is suppressed by cortisol itself, but due to hyperglycemia caused by glucocorticoids and increased insulin secretion, fat formation increases. Fat is deposited in
upper body, neck and face.
The effects on carbohydrate metabolism are generally opposite to that of insulin, which is why glucocorticoids are called contrainsular hormones. Under the influence of cortisol, hyperglycemia occurs due to: 1) increased formation of carbohydrates from amino acids through gluconeogenesis; 2) suppression of glucose utilization by tissues. The consequence of hyperglycemia is glycosuria and stimulation of insulin secretion. A decrease in cell sensitivity to insulin, combined with contrainsular and catabolic effects, can lead to the development of steroid-induced diabetes mellitus.
The systemic effects of cortisol manifest themselves as a decrease in the number of lymphocytes, eosinophils and basophils in the blood, an increase in neutrophils and red blood cells, an increase in sensory sensitivity and excitability of the nervous system, an increase in the sensitivity of adrenergic receptors to the action of catecholamines, maintaining optimal functional state and regulation of the cardiovascular system. Glucocorticoids increase the body's resistance to excessive irritants and suppress inflammation and allergic reactions, why they are called adaptive and anti-inflammatory hormones.
Excess glucocorticoids not associated with increased secretion of corticotropin is called Itsenko-Cushing syndrome. Its main manifestations are similar to Itsenko-Cushing's disease, however, thanks to feedback, the secretion of corticotropin and its level in the blood are significantly reduced. Muscle weakness, a tendency to diabetes mellitus, hypertension and sexual dysfunction, lymphopenia, peptic ulcers of the stomach, mental changes - these are far from full list symptoms of hypercortisolism.
Glucocorticoid deficiency causes hypoglycemia, decreased body resistance, neutropenia, eosinophilia and lymphocytosis, impaired adrenoreactivity and cardiac activity, and hypotension.
9. Sympatho-adrenal system, its functional organization. Catecholamines as mediators and hormones. Participation in stress. Nervous regulation of adrenal chromaffin tissue.
Catecholamines - hormones of the adrenal medulla, represented by adrenaline and norepinephrine , which are secreted in a 6:1 ratio.
Main metabolic effects. adrenaline are: increased breakdown of glycogen in the liver and muscles (glycogenolysis) due to activation of phosphorylase, suppression of glycogen synthesis, suppression of glucose consumption by tissues, hyperglycemia, increased oxygen consumption by tissues and oxidative processes in them, activation of the breakdown and mobilization of fat and its oxidation.
Functional effects of catecholamines. depend on the predominance of one of the types of adrenergic receptors (alpha or beta) in the tissues. For adrenaline, the main functional effects are manifested in the form of: increased frequency and intensification of heart contractions, improved conduction of excitation in the heart, constriction of blood vessels in the skin and abdominal organs; increasing heat generation in tissues, weakening contractions of the stomach and intestines, relaxing bronchial muscles, dilating pupils, reducing glomerular filtration and urine formation, stimulating the secretion of renin by the kidney. Thus, adrenaline improves the body’s interaction with the external environment and increases performance in emergency conditions. Adrenaline is a hormone of urgent (emergency) adaptation.
The release of catecholamines is regulated by the nervous system through sympathetic fibers passing through the splanchnic nerve. Nerve centers, regulating the secretory function of chromaffin tissue, are located in the hypothalamus.
10. Endocrine function of the pancreas. The mechanisms of action of its hormones on carbohydrate, fat, and protein metabolism. Regulation of glucose levels in the liver, muscle tissue, nerve cells. Diabetes. Hyperinsulinemia.
Sugar-regulating hormones, i.e. Many hormones of the endocrine glands influence blood sugar and carbohydrate metabolism. But the most pronounced and powerful effects are exerted by the hormones of the islets of Langerhans of the pancreas - insulin and glucagon . The first of them can be called hypoglycemic, as it reduces blood sugar levels, and the second - hyperglycemic.
Insulin has a powerful effect on all types of metabolism. Its effect on carbohydrate metabolism is mainly manifested by the following effects: it increases the permeability of cell membranes in muscles and adipose tissue for glucose, activates and increases the content of enzymes in cells, enhances the utilization of glucose by cells, activates phosphorylation processes, suppresses the breakdown and stimulates the synthesis of glycogen, inhibits gluconeogenesis , activates glycolysis.
The main effects of insulin on protein metabolism: increasing membrane permeability for amino acids, enhancing the synthesis of proteins necessary for the formation
nucleic acids, primarily mRNA, activation of amino acid synthesis in the liver, activation of synthesis and suppression of protein breakdown.
The main effects of insulin on fat metabolism: stimulation of the synthesis of free fatty acids from glucose, stimulation of triglyceride synthesis, suppression of fat breakdown, activation of ketone body oxidation in the liver.
Glucagon causes the following main effects: activates glycogenolysis in the liver and muscles, causes hyperglycemia, activates gluconeogenesis, lipolysis and suppression of fat synthesis, increases the synthesis of ketone bodies in the liver, stimulates protein catabolism in the liver, increases urea synthesis.
The main regulator of insulin secretion is D-glucose in the incoming blood, which activates a specific pool of cAMP in beta cells and, through this intermediary, leads to stimulation of the release of insulin from secretory granules. Enhances beta cell response to glucose hormone intestines - stomach inhibitory peptide (IIP). Through a nonspecific, glucose-independent pool, cAMP stimulates insulin secretion and CA++ ions. The nervous system also plays a certain role in the regulation of insulin secretion, in particular nervus vagus and acetylcholine stimulate insulin secretion, and sympathetic nerves and catecholamines through alpha-adrenergic receptors suppress insulin secretion and stimulate glucagon secretion.
A specific inhibitor of insulin production is the hormone of delta cells of the islets of Langerhans - somatostatin . This hormone is also formed in the intestines, where it inhibits the absorption of glucose and thereby reduces the response of beta cells to a glucose stimulus.
Glucagon secretion is stimulated by a decrease in blood glucose levels, under the influence of gastrointestinal hormones (GIP, gastrin, secretin, pancreozymin-cholecystokinin) and by a decrease in the content of CA++ ions, and is inhibited by insulin, somatostatin, glucose and calcium.
Absolute or relative deficiency of insulin in relation to glucagon manifests itself in the form of diabetes mellitus. With this disease, profound metabolic disorders occur and, if insulin activity is not restored artificially from the outside, death may occur. Diabetes mellitus is characterized by hypoglycemia, glucosuria, polyuria, thirst, constant feeling hunger, ketonemia, acidosis, weakness of the immune system, circulatory failure and many other disorders. An extremely severe manifestation of diabetes mellitus is diabetic coma.
11. Thyroid gland, physiological role her hormones. Hypo- and hyperfunction.
Thyroid hormones are triiodothyronine and tetraiodothyronine (thyroxine ). The main regulator of their secretion is the adenohypophysis hormone thyrotropin. In addition, there is a direct neural regulation thyroid gland via sympathetic nerves. Feedback is carried out by the level of hormones in the blood and is closed in both the hypothalamus and the pituitary gland. The intensity of secretion of thyroid hormones affects the volume of their synthesis in the gland itself (local feedback).
Main metabolic effects. thyroid hormones are: increasing the absorption of oxygen by cells and mitochondria, activation of oxidative processes and increasing basal metabolism, stimulation of protein synthesis by increasing the permeability of cell membranes for amino acids and activation of the genetic apparatus of the cell, lipolytic effect, activation of the synthesis and excretion of cholesterol with bile, activation of glycogen breakdown , hyperglycemia, increased tissue glucose consumption, increased glucose absorption in the intestine, activation of liver insulinase and acceleration of insulin inactivation, stimulation of insulin secretion due to hyperglycemia.
The main functional effects of thyroid hormones are: ensuring normal processes of growth, development and differentiation of tissues and organs, activation of sympathetic effects by reducing the breakdown of the mediator, the formation of catecholamine-like metabolites and increasing the sensitivity of adrenergic receptors (tachycardia, sweating, vasospasm, etc.), increasing heat generation and body temperature, activation of the internal nervous system and increased excitability of the central nervous system, increased energy efficiency of mitochondria and myocardial contractility, protective effect against the development of myocardial damage and ulcer formation in the stomach under stress, increased renal blood flow, glomerular filtration and diuresis, stimulation of regeneration and healing processes, ensuring normal reproductive activity.
Increased secretion of thyroid hormones is a manifestation of hyperfunction of the thyroid gland - hyperthyroidism. In this case, characteristic changes in metabolism are noted (increased basal metabolism, hyperglycemia, weight loss, etc.), symptoms of excessive sympathetic effects (tachycardia, excessive sweating, increased excitability, increased blood pressure, etc.). Maybe
develop diabetes.
Congenital deficiency of thyroid hormones impairs the growth, development and differentiation of the skeleton, tissues and organs, including the nervous system (occurs mental retardation). This congenital pathology called "cretinism". Acquired thyroid deficiency or hypothyroidism manifests itself in a slowdown of oxidative processes, a decrease in basal metabolism, hypoglycemia, degeneration of subcutaneous fat and skin with the accumulation of glycosaminoglycans and water. The excitability of the central nervous system decreases, sympathetic effects and heat production are weakened. The complex of such disorders is called “myxedema”, i.e. mucous swelling.
Calcitonin - Produced in parafollicular K cells of the thyroid gland. The target organs for calcitonin are bones, kidneys and intestines. Calcitonin reduces calcium levels in the blood by facilitating mineralization and inhibiting bone resorption. Reduces the reabsorption of calcium and phosphate in the kidneys. Calcitonin inhibits the secretion of gastrin in the stomach and reduces the acidity of gastric juice. The secretion of calcitonin is stimulated by an increase in the level of Ca++ in the blood and gastrin.
12. Parathyroid glands, their physiological role. Maintenance Mechanisms
concentrations of calcium and phosphate in the blood. The importance of vitamin D.
The regulation of calcium metabolism is carried out mainly due to the action of parathyrin and calcitonin. Parathyroid hormone, or parathyrin, parathyroid hormone, is synthesized in the parathyroid glands. It ensures an increase in calcium levels in the blood. The target organs for this hormone are bones and kidneys. In bone tissue, para-thyrine enhances the function of osteoclasts, which promotes bone demineralization and increases the level of calcium and phosphorus in the blood plasma. In the tubular apparatus of the kidneys, parathyrin stimulates the reabsorption of calcium and inhibits the reabsorption of phosphates, which leads to hypercalcemia and phosphaturia. The development of phosphaturia may have a certain significance in the implementation of the hypercalcemic effect of the hormone. This is due to the fact that calcium forms insoluble compounds with phosphates; therefore, increased excretion of phosphates in the urine helps to increase the level of free calcium in the blood plasma. Parathyrine enhances the synthesis of calcitriol, which is an active metabolite of vitamin D 3 . The latter is initially formed in an inactive state in the skin under the influence ultraviolet radiation, and then, under the influence of parathyrin, its activation occurs in the liver and kidneys. Calcitriol enhances the formation of calcium-binding protein in the intestinal wall, which promotes reverse suction calcium and the development of hypercalcemia. Thus, the increase in calcium reabsorption in the intestine during parathyrin overproduction is mainly due to its stimulating effect on the activation processes of vitamin D 3 . The direct effect of parathyrin itself on the intestinal wall is very insignificant.
When the parathyroid glands are removed, the animal dies from tetanic convulsions. This is due to the fact that in the case of low calcium levels in the blood, neuromuscular excitability sharply increases. In this case, the action of even minor external stimuli leads to muscle contraction.
Overproduction of parathyrin leads to demineralization and resorption of bone tissue, the development of osteoporosis. The level of calcium in the blood plasma increases sharply, resulting in an increased tendency to stone formation in organs genitourinary system. Hypercalcemia contributes to the development of severe disturbances in the electrical stability of the heart, as well as the formation of ulcers in digestive tract, the occurrence of which is due to the stimulating effect of Ca 2+ ions on the production of gastrin and of hydrochloric acid in the stomach.
The secretion of parathyrin and thyrocalcitonin (see section 5.2.3) is regulated by negative feedback depending on the level of calcium in the blood plasma. With a decrease in calcium levels, the secretion of parathyrin increases and the production of thyrocalcitonin is inhibited. Under physiological conditions, this can be observed during pregnancy, lactation, and reduced calcium content in food intake. An increase in the concentration of calcium in the blood plasma, on the contrary, helps to reduce the secretion of parathyrin and increase the production of thyrocalcitonin. The latter may have great importance in children and persons young, since at this age the formation of the bone skeleton occurs. Adequate occurrence of these processes is impossible without thyrocalcitonin, which determines the absorption of calcium from the blood plasma and its inclusion in the structure of bone tissue.
13. Sex glands. Functions of female sex hormones. Menstrual-ovarian cycle, its mechanism. Fertilization, pregnancy, childbirth, lactation. Endocrine regulation of these processes. Age-related changes in hormone production.
Male sex hormones .
Male sex hormones - androgens - are formed in Leydig cells of the testes from cholesterol. The main androgen in humans is testosterone . . Small amounts of androgens are produced in the adrenal cortex.
Testosterone has wide range metabolic and physiological effects: ensuring differentiation processes in embryogenesis and the development of primary and secondary sexual characteristics, the formation of central nervous system structures that ensure sexual behavior and sexual functions, generalized anabolic effect, ensuring the growth of skeleton, muscles, distribution of subcutaneous fat, ensuring spermatogenesis, retention of nitrogen, potassium, phosphate in the body, activation of RNA synthesis, stimulation of erythropoiesis.
Androgens are also produced in small quantities in female body, being not only precursors for the synthesis of estrogen, but also supporting libido, as well as stimulating hair growth in the pubis and armpits.
Female sex hormones .
The secretion of these hormones ( estrogen) is closely related to the female reproductive cycle. The female reproductive cycle ensures clear integration over time of various processes necessary for reproductive function - periodic preparation of the endometrium for embryo implantation, egg maturation and ovulation, changes in secondary sexual characteristics, etc. Coordination of these processes is ensured by fluctuations in the secretion of a number of hormones, primarily gonadotropins and sex hormones steroids. The secretion of gonadotropins is carried out as “tonic”, i.e. continuously and “cyclically”, with periodic release of large quantities of folliculin and luteotropin in the middle of the cycle.
The sexual cycle lasts 27-28 days and is divided into four periods:
1) preovulatory - the period of preparation for pregnancy, the uterus at this time increases in size, the mucous membrane and its glands grow, the contraction of the fallopian tubes and the muscular layer of the uterus intensifies and becomes more frequent, the vaginal mucosa also grows;
2) ovulatory- begins with the rupture of the vesicular ovarian follicle, the release of the egg from it and its movement along fallopian tube into the uterine cavity. During this period, fertilization usually occurs, the sexual cycle is interrupted and pregnancy occurs;
3) post-ovulation- in women during this period, menstruation appears, the unfertilized egg, which remains alive in the uterus for several days, dies, tonic contractions of the muscles of the uterus increase, leading to the rejection of its mucous membrane and the release of fragments of the mucous membrane along with blood.
4) rest period- occurs after the end of the post-ovulation period.
Hormonal changes during the sexual cycle are accompanied by the following changes. In the preovulation period, first there is a gradual increase in the secretion of follitropin by the adenohypophysis. The maturing follicle produces everything large quantity estrogen, which, through feedback, begins to reduce the production of follinotropin. An increasing level of lutropin leads to stimulation of the synthesis of enzymes, leading to thinning of the follicle wall necessary for ovulation.
During the ovulation period, there is a sharp surge in the level of lutropin, follitropin and estrogens in the blood.
In the initial phase of the postovulation period, there is a short-term drop in the level of gonadotropins and estradiol , the ruptured follicle begins to fill with luteal cells, and new blood vessels are formed. Products are increasing progesterone the resulting corpus luteum, the secretion of estradiol by other maturing follicles increases. The resulting level of progesterone and estrogen feedback suppresses the secretion of follotropin and luteotropin. Degeneration of the corpus luteum begins, the level of progesterone and estrogen in the blood drops. In the secretory epithelium without steroid stimulation, hemorrhagic and degenerative changes, which leads to bleeding, rejection of the mucous membrane, contraction of the uterus, i.e. to menstruation.
14. Functions of male sex hormones. Regulation of their formation. Pre- and postnatal effects of sex hormones on the body. Age-related changes in hormone production.
Endocrine function of the testes.
1) Sertoli cells - produce the hormone inhibin - inhibits the formation of follitropin in the pituitary gland, the formation and secretion of estrogens.
2) Leydig cells - produce the hormone testosterone.
- Provides differentiation processes in embryogenesis
- Development of primary and secondary sexual characteristics
- Formation of central nervous system structures that ensure sexual behavior and functions
- Anabolic effect (growth of skeleton, muscles, distribution of subcutaneous fat)
- Regulation of spermatogenesis
- Retains nitrogen, potassium, phosphate, calcium in the body
- Activates RNA synthesis
- Stimulates erythropoiesis.
Endocrine function of the ovaries.
In the female body, hormones are produced in the ovaries and hormonal function possess cells of the granular layer of follicles, which produce estrogens (estradiol, estrone, estriol) and cells of the corpus luteum (produce progesterone).
Functions of estrogen:
- Provide sexual differentiation in embryogenesis.
- Puberty and development of female sexual characteristics
- Establishment of the female reproductive cycle, growth of uterine muscles, development of mammary glands
- Determine sexual behavior, oogenesis, fertilization and implantation into eggs
- Development and differentiation of the fetus and the course of labor
- Suppress bone resorption, retain nitrogen, water, and salts in the body
Functions of Progesterone:
1. Suppresses contraction of the uterine muscles
2. Necessary for ovulation
3. Suppresses gonadotropin secretion
4. Has an antialdosterone effect, i.e. it stimulates natriuresis.
15. Thymus gland (thymus), its physiological role.
The thymus gland is also called the thymus or thymus gland. It, like the bone marrow, is the central organ of immunogenesis (immune formation). The thymus is located directly behind the sternum and consists of two lobes (right and left), connected by loose fiber. The thymus is formed earlier than other organs immune system, its weight in newborns is 13 g, greatest mass- about 30 g - the thymus is present in children 6-15 years old.
Then it undergoes reverse development (age-related involution) and in adults is almost completely replaced by fatty tissue (in people over 50 years of age adipose tissue makes up 90% of the total mass of the thymus (on average 13-15 g)). The period of greatest activity is associated with the activity of the thymus intensive growth body. The thymus contains small lymphocytes (thymocytes). The decisive role of the thymus in the formation of the immune system became clear from experiments conducted by the Australian scientist D. Miller in 1961.
He found that removal of the thymus in newborn mice leads to a decrease in the production of antibodies and an increase in the lifespan of the transplanted tissue. These facts indicated that the thymus takes part in two forms of immune response: in humoral type reactions - the production of antibodies and in cellular type reactions - rejection (death) of transplanted foreign tissue (graft), which occur with the participation of different classes of lymphocytes. The so-called B lymphocytes are responsible for the production of antibodies, and T lymphocytes are responsible for transplant rejection reactions. T and B lymphocytes are formed through various transformations of stem cells bone marrow.
Penetrating from it into the thymus, stem cell transforms under the influence of hormones of this organ, first into the so-called thymocyte, and then, entering the spleen or The lymph nodes, - into an immunologically active T-lymphocyte. The transformation of a stem cell into a B lymphocyte appears to occur in the bone marrow. In the thymus gland, along with the formation of T-lymphocytes from bone marrow stem cells, hormonal factors- thymosin and thymopoietin.
Hormones that ensure differentiation (distinction) of T-lymphocytes and play a certain role in cellular immune reactions. There is also evidence that hormones ensure the synthesis (construction) of certain cellular receptors.
Hormones are organic substances that affect metabolic processes, the functioning of tissues and organs, and the growth of the body. They are produced in humans by the endocrine glands, enter the blood or lymph and are delivered to target cells, which they influence.
Glands
They are called endocrine (internal secretion) because they do not have ducts to the outside, their secretion (hormones) remains inside the body. They regulate each other’s work and are able to accelerate or slow down the rate of hormone production, thereby affecting the functioning of all organs and tissues. We can say that the entire vital activity of the body rests on them. The endocrine glands include:

They perform various functions.
Pituitary gland and hypothalamus
This system is located in the occipital part of the brain, despite its small size(only 0.7 g), it is the “head” of the whole. Most of the hormones produced by the pituitary gland regulate the functioning of other glands. The hypothalamus functions as a “sensor”, picking up signals from the brain about fluctuations in the level of other hormones, and sending a “command” to the pituitary gland that it is time to start working. Previously, it was also considered a full-fledged gland that influenced the functioning of the body, but thanks to research it was found that hormones are secreted by the pituitary gland, and the hypothalamus regulates these functions through releasing hormones. There are two types of them: some start the secretion process (releasing), others inhibit (stopping). TO pituitary hormones include:

Thyroid and parathyroid glands
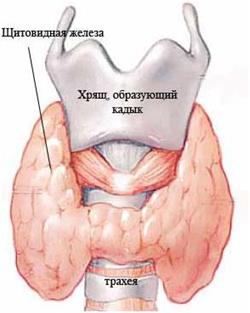 The thyroid gland is located in the area of the upper third of the trachea, attaching to it connective tissue, has two lobes and an isthmus, resembling an inverted butterfly in shape. Average weight its about 19 gr. The thyroid gland secretes thyroid hormones: thyroxine and triiodothyronine, which are involved in cellular metabolism and energy exchange. Maintaining human body temperature, maintaining the body during stress and physical activity, the cells receiving water and nutrients, the formation of new cells - all this is the activity of thyroid hormones.
The thyroid gland is located in the area of the upper third of the trachea, attaching to it connective tissue, has two lobes and an isthmus, resembling an inverted butterfly in shape. Average weight its about 19 gr. The thyroid gland secretes thyroid hormones: thyroxine and triiodothyronine, which are involved in cellular metabolism and energy exchange. Maintaining human body temperature, maintaining the body during stress and physical activity, the cells receiving water and nutrients, the formation of new cells - all this is the activity of thyroid hormones.
On back wall The thyroid gland contains small (no more than 6 g) parathyroid glands. Most often, a person has two pairs of them, but sometimes there are fewer, which is considered a variant of the norm. They produce hormones that regulate the level of calcium in the blood - paratin. They act in tandem with calcitonin, a thyroid hormone that lowers calcium levels, and they increase it. 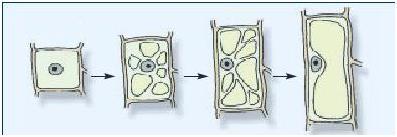
This is an unpaired small organ located between the hemispheres in the center of the brain. Its shape resembles a pine cone, for which it received its second name - pineal body. Weight is only 0.2 g. The activity of this gland depends on the illumination of the place where the person is. His leashes are attached to optic nerves, through them he receives signals. In light it produces serotonin, in darkness it produces melatonin.
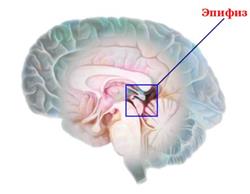 Serotonin also plays the role of a neurotransmitter - a substance that promotes the transmission of impulses between neurons, thanks to this property it improves a person’s mood, restrains impulses from the feeling of pain, and is responsible for muscle activity.
Serotonin also plays the role of a neurotransmitter - a substance that promotes the transmission of impulses between neurons, thanks to this property it improves a person’s mood, restrains impulses from the feeling of pain, and is responsible for muscle activity.
Once in the blood, it performs the functions of a hormone: it affects the development inflammatory processes and blood clotting, slightly on allergic reactions and regulates the functioning of the hypothalamus.
Melatonin is a hormone derived from serotonin and is responsible for blood pressure, falling asleep and depth of sleep, activates the immune system, inhibits the synthesis of somatotropic hormone, reducing the risk of tumor development, controls puberty and sexual arousal. During sleep, it restores damaged cells and inhibits the aging process. That’s why healthy, good sleep is so important for a person.
 The pineal gland produces another hormone - adrenoglomerulotropin, its functions are not yet clear, scientists managed to find out that it affects the secretion of hormones by the adrenal medulla, but the whole process remains a mystery to them.
The pineal gland produces another hormone - adrenoglomerulotropin, its functions are not yet clear, scientists managed to find out that it affects the secretion of hormones by the adrenal medulla, but the whole process remains a mystery to them.
It is located behind the sternum and is a paired organ weighing about 20 grams. It grows until puberty, then begins to slowly atrophy; in older people it is almost indistinguishable from adipose tissue. Thymus - important organ immune system, in which T cells mature, differentiate, and are immunologically “trained.” It produces hormones:
- Timalin;
- Thymosin;
- Thymopoietin;
- IGF-1;
 Its role for the body has not yet been sufficiently studied. But its most important function is to prevent a person from dying from infections in childhood. It works hard in babies, producing T-lymphocytes, giving them T cell receptors and co-receptors (markers), forming acquired immunity. It is thanks to the thymus that a person does not get sick twice with diseases caused by measles viruses, chickenpox, rubella and many others.
Its role for the body has not yet been sufficiently studied. But its most important function is to prevent a person from dying from infections in childhood. It works hard in babies, producing T-lymphocytes, giving them T cell receptors and co-receptors (markers), forming acquired immunity. It is thanks to the thymus that a person does not get sick twice with diseases caused by measles viruses, chickenpox, rubella and many others.
They are located above each of the human kidneys, one weighs about 4 g, 90% of the gland is the adrenal cortex, the remaining 10% is the medulla. They produce various groups hormones:
- Mineralocorticoids (water-salt balance);
- Glucocorticoids (glucose formation, anti-shock effect, immunoregulation, antiallergic effect);
- Androgens (protein synthesis and breakdown, glucose utilization, lowering cholesterol and lipids in the blood, reducing the amount of subcutaneous fat);
- Catecholamines (support the body during fear, rage, physical exertion, signaling the hypothalamus to strengthen the work of other glands);
- Peptides (cell regeneration, removal of toxins, increases tissue wear resistance).
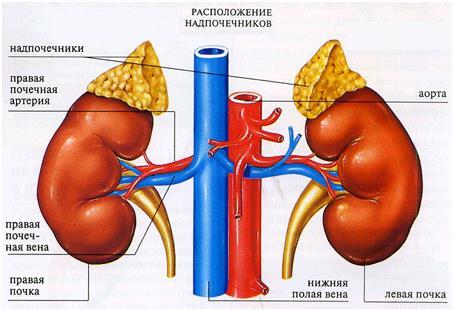
It is located in the epigastric region, behind the stomach. Endocrine functions performs only a small part of it - the pancreatic islets. They are not located in one place, but are scattered unevenly throughout the gland. They secrete several hormones:
- Glucagon (increases blood glucose levels);
- Insulin (transportation of glucose into cells).
Most of the pancreas produces gastric juices, performing an exocrine function. 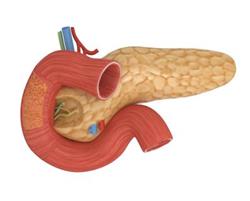
The sex glands include the testes and ovaries; they, like the pancreas, are mixed glands, performing intrasecretory and exocrine functions.
Ovaries - paired female glands, located in the pelvic cavity, weight about 7 grams. They produce steroid hormones: estrogens, gestagens, androgens. They ensure ovulation and the formation of the corpus luteum after conception. Their concentration is not constant, one of the hormones dominates, then another and a third, which creates a cycle.
The testicles are also a paired male organ; the glands are located in the scrotum. The main hormone of the testes is testosterone.
The gonads are responsible for the development of the genital organs and the maturation of the egg and sperm. They form secondary sexual characteristics: voice timbre, skeletal structure, location of fat deposits and hair, influence mental behavior - everything that distinguishes men from women.
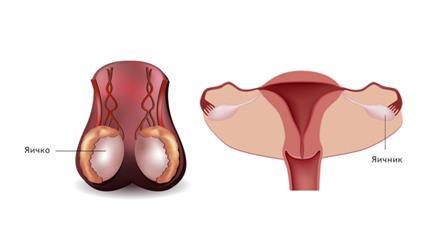 All glands have an increased blood supply to nearby aortas or arteries, which once again emphasizes the importance of the production and rapid delivery of hormones to the corresponding cells.
All glands have an increased blood supply to nearby aortas or arteries, which once again emphasizes the importance of the production and rapid delivery of hormones to the corresponding cells.
The complete absence of one of the glands will lead to disruption of the others or death. Doctors managed to completely replace medicines only thyroid hormones.
Related posts:
Add a comment

